Cancer-related fatigue (CRF) is one of the most common, severe and distressing symptoms reported by young people regardless of their diagnosis or treatment. Here we unpack the causes, signs and symptoms of CRF, and what can be done to help.
HOW IT DIFFERS FROM TIREDNESS
CRF is often confused with tiredness, but it is very different. Tiredness happens to everyone- it is the feeling you expect after performing certain activities or at the end of the day, and is resolved by a good night’s sleep. CRF on the other hand, does not result from activity, exertion or staying up late, and is not relieved by sleep. It can come on suddenly and fluctuate in severity from hour-to-hour, day-to-day, week-to-week.
COMMON SIGNS AND SYMPTOMS
There is no one simple way to tell if you have CRF because it is invisible and presents differently for each person. However, it is often defined as a whole body exhaustion which can affect how you think, feel, behave and move. It can include:
- Difficulty staying focused - this can make it hard to stay on task during class or lectures or to read relatively simple information
- Challenges with problem solving and organisation - this may include difficulty with starting or prioritising tasks
- Trouble remembering information and thinking of the right word or name - this tends to happen when put on the spot or in front of people, which can be embarrassing
- Low motivation or mood - this can include feeling sad, frustrated and irritable
- Feeling weak or heavy - this can make taking a shower feel like an impossible task

HOW COMMON IS CRF AND HOW LONG DOES IT LAST?
Research has found that over 50% of young people experience CRF. It fluctuates in severity and can persist for many years after treatment, with some perceiving it to be worse more than one year after completing treatment. However, just like signs and symptoms, this varies greatly between individuals.
Please feel reassured, though, that CRF usually improves with time and there is plenty you can do to reduce the impact it has on your life (we’ll get to that later in this topic!)
CAUSES OF CRF
CRF is often caused by a number of factors, which can include:
- Cancer itself - for example, due to chemical or hormonal changes linked to inflammatory processes that alter energy needs
- Side effects of treatment or medications - such as or pain
- Emotional changes - such as anxiety, stress, depression or loss of confidence
- Inadequate sleep, nutrition and exercise
- Fatigue itself can also exacerbate fatigue - it can create a vicious cycle as fatigue often hinders your ability to exercise and perform activities, leading to reduced fitness and strength, which can in turn worsen fatigue

IS CRF DIFFERENT IN YOUNG PEOPLE?
Compared to older adults, young people with a cancer experience may be at greater risk for or have more severe CRF. This is unsurprising given even healthy young people experience fatigue as they undergo the rapid characteristic of this life stage. All these changes mean a need for more sleep, but this often doesn’t happen due to and the development of that can be unhelpful for sleep.
CRF is thought to be particularly distressing for young people as it can hinder independence and the ability to engage in activities that are really important at this age, such as attending school or work, being active and socialising with friends.
STRATEGIES FOR DEALING WITH CRF
There is no quick fix for CRF, but it usually improves over time and there are plenty of things you can do to help reduce the impact it has on your daily life. Some key strategies are discussed below.

1. Seek support from your healthcare team
CRF can be complex and early intervention is important to reduce the impact it can have on your life, so discuss how you are feeling or any concerns you have with your GP or treating team as soon as possible. They will be able to provide you with direct support and/or refer you to specialist services such as the following, who can help in a variety of ways:
- Exercise physiologists and physiotherapists
- Dietitians
- Social workers and psychologists
- Occupational therapists
2. Exercise regularly
Exercise and physical activity improves CRF in several ways. It helps break the fatigue cycle by increasing strength and fitness, and improves sleep and emotional wellbeing.
The irony is that exercise is often the last thing that people with CRF feel like doing. Fortunately there are healthcare professionals (namely exercise physiologists and physiotherapists) and a range of strategies that can assist you with resuming or commencing exercise and physical activity. These strategies are outlined in the topic on ‘Exercise & Getting Active’, but some simple ones specific to fatigue include:
|
Prioritise
|
|
|
Plan
|
|
|
Pace
|
|
|
Progress
|
|
|
Patience
|
|
3. Eat a balanced, nutritious diet
Eating a well-balanced, nutritional diet and ensuring you remain hydrated can make a huge difference to your energy levels, but this can be challenging given cancer and its treatment can affect your dietary habits, appetite, swallowing and sense of taste and smell. The ‘Diet & Nutrition’ topic provides some recommendations to assist you with overcoming these challenges and dietitians can provide you with tailored advice if needed.
4. Take care of your emotional health and wellbeing
Many young people with cancer experience a range of concerns that can affect their emotional health and wellbeing which may contribute to CRF. It is important to address these practical and emotional concerns and develop effective coping strategies. The ‘Emotional Health & Wellbeing’ topic offers plenty of advice, and healthcare professionals such as social workers and psychologists can provide you with individualised support.
5. Manage changes in thinking and memory
CRF is linked to cognitive challenges such as problems with concentration and attention, following conversations, and remembering the right word or someone’s name. Many young people find this quite distressing and frustrating, but it usually improves within the first year following treatment, and your healthcare team can provide strategies to assist. You may also find this resource helpful.
6. Communicate your needs
Getting the support you need is so important given the significant impact CRF can have on your life. Talk to your healthcare team, but discuss how you are feeling with others as well- this may include your parents, friends, teachers, lecturers or managers.
It’s common to feel uncomfortable or uncertain with how to start a discussion or what you should say- the topics on ‘Relationships’ and ‘School, Study & Work’ provide some suggestions and your healthcare team can also provide guidance.
7. Conserve your energy
It’s important that you spend your energy on the tasks and activities that you want and need to perform. It’s also important that you don’t overdo it as this may completely deplete your energy stores and leave you feeling exhausted. The Triple P approach outlined below can be useful.
Occupational therapists can also provide advice on a range of other fatigue management strategies that are specific to your needs.

- Write a list of tasks that you need to complete each day and week
- Establish when your energy levels are highest
- Write a list of tasks that you need to complete each day and week
- Establish when your energy levels are highest
- Write a list of tasks that you need to complete each day and week
- Establish when your energy levels are highest
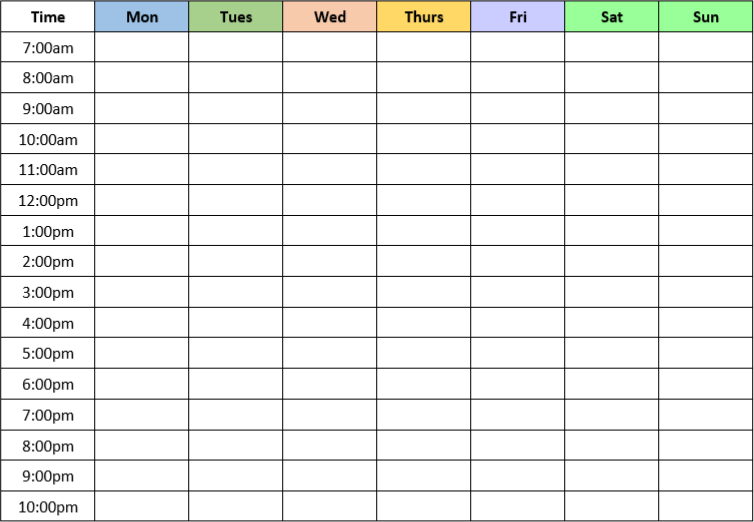
8. Develop a daily routine
Our bodies respond extremely well to daily structure and routine. It assists with regulating our , reducing stress, improving sense of control and coping with change. The significant disruption to routine that cancer often causes can continue well after treatment ends, particularly if you have not yet returned to study or work.
To get your routine back on track, it can be helpful to develop a weekly timetable that includes the tasks and activities you need to finish each day and by end of the week. There are many great calendar and planning apps you can use for this, or you might prefer a paper-based version that looks something like this one, posted in a clearly visible place:
9. Practice good sleep hygiene
Just like daily routines, our bodies respond extremely well to regular sleep habits. This includes going to bed and waking up at the same time every day (weekends too, and even if you had a poor night’s sleep), which helps with setting your .
Exposure to light also assists with setting our body clock. Natural light in the morning can help us to feel alert and softer light at night can assist with relaxation and preparing our bodies for sleep.
Developing good sleep habits (known as sleep hygiene) can be hard at first, as it usually takes at least 2 months before a new behaviour becomes automatic. However, it is worth persisting as you will almost certainly see and feel the benefits. There is also a range of healthcare professionals (including GPs, psychologists and occupational therapists) who can assist you if needed.
BEFORE BEDTIME:
- Avoid alcohol, cigarettes and stimulants (which include coffee, tea, chocolate, soft drinks, energy drinks) after lunchtime
- Avoid high intensity exercise approximately 3 hours prior to bedtime
- Spend some time writing down any of your concerns or worries (preferably at least 2 hours before bedtime) given they often arise and appear far worse in the middle of the night- you can then review in the morning and raise with family, friends or healthcare professionals if needed
ESTABLISH A PRE-BEDTIME RITUAL:
- Have a shower or bath 1-2 hours before bedtime as this raises body temperature which creates sleepiness once it drops back down again
- Set an alarm for approximately 30 minutes before you want to be in bed to commence preparation - this may include brushing your teeth (this can often wake you up if you do it immediately before bed) and turning on your bedside light so you don’t have to enter a bright room
- Practice relaxation, meditation or mindfulness - you may need to try a few approaches to find the one that is right for you. These apps and resources are all great places to start: Smiling Mind, Headspace, Calm, Insight Timer.
CREATE THE RIGHT SLEEP ENVIRONMENT:
- Ensure your bedroom is dark, quiet and cool (ideally around 18 degrees)
- A comfortable bed and pillow is important
ONCE IN BED:
- Try to avoid electronic devices like phones and tablets if possible - that said, they can be a useful source of relaxation and distraction, so if using, dim their brightness and avoid things that will make you alert
- Ban yourself from clock-watching - this will likely make you feel stressed and reinforce negative thoughts (“Gaah, look how late it is, I’ll never get to sleep and will feel terrible tomorrow!”)
- If you’re not asleep after 20-30 minutes, move to another room and do something relaxing until you feel sleepy
USEFUL LINKS AND RESOURCES
There is a lot of information about fatigue out there given it is one of the most common side effects of cancer and its treatment.
It’s important to remember that cancer-related fatigue varies greatly between individuals in terms of causes and impacts, so what you read may not match what you are experiencing, or be relevant to your circumstances. It can also be difficult to determine how reputable some information sources truly are.
It is always best to discuss any concerns you have with your GP or treating team- they will be able to tailor information, resources and strategies to your specific needs and circumstances.
- Your local youth cancer service – each Australian state has a team of health care professionals specialising in the cancer treatment and care of young people aged 15-25 that you can contact for help and advice
- Sleep and young people (Headspace) – sleep myths, truths and tips for young people specifically
- Dealing with cancer-related fatigue (Australian Cancer Survivorship Centre) – good summary of CRL and how it can be managed
- Cancer fatigue: live better (Peter MacCallum Cancer Centre) – general info with a focus on monitoring your fatigue and its level of severity